When an infectious disease strikes, every day matters. The longer it takes to spot, investigate, and contain an outbreak, the more lives we may lose.
That is why we must prepare our public-health data systems for the next pandemic and revamp them to tackle the current one. COVID-19 is far from over; in many countries, it is getting worse. By investing in digital technologies now and publishing anonymized data online, policymakers can strengthen their response to the ongoing pandemic, and act quickly when another public-health threat appears.
An important first step toward more robust pandemic preparedness is reporting of hospitals’ admissions data to national health officials as patients arrive. An unusually large number of admissions, even in the absence of laboratory testing, could be the first warning sign of a deadly new threat. Reporting admissions data together with diagnoses, such as pneumonia, can enhance the value of this stream of daily data, and potentially enable public-health officials to nip the next pandemic in the bud.
Countries should also build systems that enable laboratories to report their results in real time. After the 2002 SARS epidemic, China invested heavily in an infectious-disease reporting system linking all hospitals in the country directly to central health authorities. This allowed officials to view lab results and diagnoses immediately. Chinese public-health officials have previously used the system to investigate and contain outbreaks of avian influenza (information that could be even more valuable if the Chinese authorities shared it with the rest of the world).
This arrangement is not perfect. When the SARS-CoV-2 virus that causes COVID-19 first emerged in China, the system broke down when local health officials delayed reporting. Still, digitizing and linking infectious-disease reporting systems is a wise investment, and will give countries a better shot at detecting the next pandemic.
Moreover, at a time when it had fewer resources than today, China created a far more advanced rapid nationwide data system than those in some wealthier countries. This is just one example of how low- and middle-income countries can leapfrog richer ones with digital technology.
But even as we think about preparing for the next pandemic, the current one is accelerating. We need to embrace digital technologies now to improve our response to COVID-19.
For starters, digitizing COVID-19 hospital admissions and laboratory data would help decision-makers identify and respond to surges faster, potentially saving more lives and preventing the need for full lockdowns. In many countries, manual reporting tends to slow to a trickle – potentially causing deadly delays – when overburdened hospital staff take much-needed time off on weekends and national holidays.
Next, we need to do more to understand how well COVID-19 treatments and vaccines are working, but we still lack the aggregate information we need to answer these questions. Countries should immediately start tracking people who receive certain therapies and vaccines. After controlling for age, sex, body-mass index, and other factors that influence a person’s risk of developing severe COVID-19, we can use treatment data to understand whether therapies are improving patients’ health. Likewise, vaccination data can help us to measure vaccines’ effectiveness and assess how long their protection lasts.
Public-health authorities also need to record and digitize key data to reduce inequity. In many countries, COVID-19 has hit racial and ethnic-minority communities especially hard, owing to systemic racism that disproportionately limits these communities from accessing high-quality health care, and makes them more likely to be essential workers at high risk for developing severe COVID-19. With much of the world’s population still unvaccinated, the spread of new, more infectious coronavirus variants threatens to deepen this disproportionate impact. Addressing the consequences of past and current mistreatment of these groups – including inequities in housing, education, employment, food, and justice – is therefore crucial, particularly when it comes to ensuring access to health information, testing, vaccination, and quality care.
On the data front, it is critical to collect information on the race, ethnicity, age, sex, postal code, and underlying health conditions of those infected with COVID-19, along with data on health outcomes. This will enable public-health leaders to distribute resources where they are needed most and assess the impact of programs designed to reduce inequalities. For countries where recording data on race and ethnicity is prohibited, educational-attainment and income data could be useful for highlighting inequities during this and future pandemics.
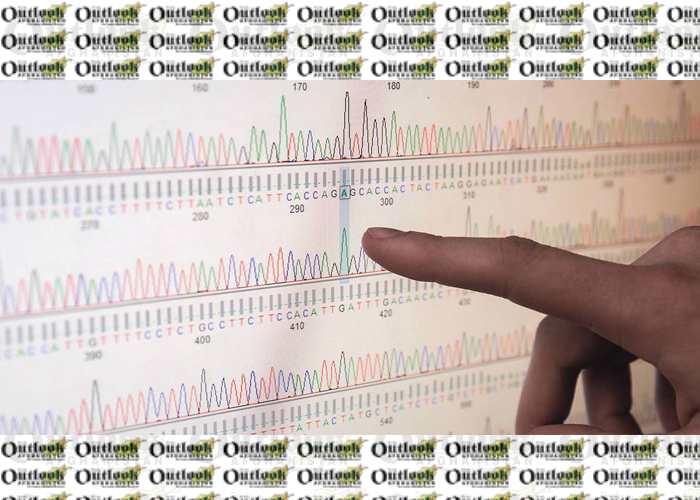
Lastly, building up capacity to carry out extensive genomic sequencing could help the world to stay ahead of the virus. Sequencing data tell us how the virus is mutating, giving us a blueprint for modifying COVID-19 vaccines as needed. As the last four months have shown, more transmissible variants, and variants that evade a person’s immunity resulting from past infection or vaccination, are changing the pandemic’s trajectory. Better genomic-sequencing data, provided in real time, can help decision-makers figure out where funding, vaccinations, and hospital support are needed most.
High-income countries should seek to emulate the United Kingdom, which has built up a large genomic-sequencing system and shares the data freely online. The Africa Centres for Disease Control and Prevention’s Africa Pathogen Genomics Initiative, which is creating a continent-wide infectious-disease reporting system and laboratory network focused on genomic sequencing, could be a useful model for low-income economies. Countries can also use genomic-sequencing data to identify COVID-19 outbreaks and understand their origins, helping to pinpoint super-spreader events and the locations where transmission occurs most frequently.
Faster and more detailed public-health data can give us a road map to navigate the remaining stages of this pandemic and be better prepared the next time a virus like SARS-CoV-2 arrives, or an even deadlier one emerges. No investment is more important.
Home » Opinion » The Public-Health Data Systems We Need
The Public-Health Data Systems We Need
| Christopher J.L. Murray